 |
Imitating and benefiting from Nature's design |
|
Imitating and benefiting from Nature's design
The design
The development of the ÆQUOS G1 knee system is based on an entirely new principle, which takes its cues from the anatomical structures and biomechanical function developed by Nature. The aim and motivation was to reproduce normal knee function as closely as possible:
|
|
Rolling followed by sliding motion (AP-translation, roll back)
Built-in protection from over-stretching
Axial rotation
Abduction/adduction
|
The ÆQUOS G1 knee joint represents a tri-compartmental total replacement prosthesis, which is intended for patients who are eligible for a bi-condylar surface joint.
|
In the case of bicondylar surface joints, which lack posterior stabilization, the ligaments (posterior cruciate and collateral ligaments) must be intact and the malformations (such as knock knees or bandy legs) should not be severe. The anterior cruciate ligament, if still present, gets resected.
A kinematic model of joint movement was developed based on the rolling-sliding motion in the normal knee. This motion is a result of the asymmetric tibial joint surfaces and the special arrangement of the femoral condyles. The link quadrangle generates the motion sequence of rolling followed by sliding.
|
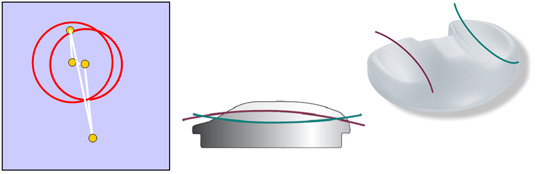 |
The joint surfaces of the ÆQUOS G1 knee endoprosthesis have basically the same morphology of curvature as the normal knee joint. Sagittally, the medial tibial surface is concave, while the lateral one is convex. The lateral femoral condyle lies further posterior to the medial one. The normal slope of 4-7 deg is part of the design of the tibial implant.
In the presence of compressive loads, the joint is best described in the sagittal plane as a link quadrangle, which brings about a rolling-sliding motion that closely resembles the situation in the natural knee. The surfaces are shaped in a way that the rolling motion mediates more than 95% of the knee movement during flexion in the range between 0 deg and 30 deg. As a result, the static friction and the shearing forces that are generated at the turnaround points (from flexion to extension and vice versa), which would otherwise lead to significant wear and tear of the polyethylene, are kept at a minimum.
|
|
The figure shows the computed kinematics of the ÆQUOS G1 prosthesis
|
The animation (see below) illustrates the marked differences in the movement trajectories between a) the ÆQUOS G1 and b) a “sliding-only” knee prosthesis:
|
|
The anterior joint junction of the TFJ widens in time to make space for the patella, coming to a rest posteriorly in the valley of the femur. As a result, the patella is protected from harmful bending torques. At the same time, the patella slides safely in the tracks of the femoral prosthesis, minimizing the chance of luxation. The quad muscles are not overly stretched and remain within their dynamic range.
Beyond 30 deg the rolling motion declines and sliding takes over.
The main function of the sliding motion is to prevent the tibia from being end-stopped on the dorsal side of the femur, allowing for larger flexions.
|
ÆQUOS ™ G1 (a) |
Conventional knee endoprosthesis (b) |
The ÆQUOS G1 knee prosthesis is characterized by a significant roll back in the tibial joint surfaces. As a result, the compressive loads that are generated during a gait cycle are spread over a large area. The medial tibial contact surface is 65,9mm² and the lateral one, 52,0mm².
|
Optical measurement of the tibial contact points using pressure-sensitive film (main axes a1 = 8.0 mm and b 1 = 2.1 mm (lateral) and a m = 9.2 mm and b m = 2.3 mm (medial); the posterior contact points indicate the roll back)
|
The ÆQUOS G1 incorporates the protective principle of self-inhibition to prevent overstretching. The kinematics of the link quadrangle prevent the joint from overstretching beyond 4 deg and ensure that the inhibition is springing and not abrupt.
IMA Dresden – Tribological studies and results
IMA GmbH in Dresden was in charge of approval testing and rating in accordance with the regulations as defined by the IMA-PV C/26 code, which corresponds to the ISO 14243-1 standard. The test procedures called for quantifying the wear and tear on the tibial inlay, as well as assessing surface quality after more than a million gait cycles. This provides standardized measures for joint durability.
Details of methods:
|
|
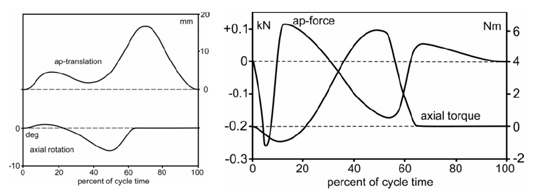
Experimental setup: The servo-hydraulic testing device Minibionix 858 was manufactured by MTS. It can be used to simulate the following four degrees of freedom: angle of flexion, axial load, axial rotation and anterior/posterior displacement of the tibia. The test series was carried out according to IMA-PV C/26, which is equivalent to the ISO/WC 14243-3 standard. The figures below indicate the trajectories of the loads and motions. The Instron-Stanmore KS4 knee simulator was developed specifically to comply with the ISO 14243-1 standard. It can also simulate four degrees of freedom: angle of flexion and axial load just as the Minibionix 858 does, and also anterior/posterior force and axial torque.
Since no apparatus exists that would allow simulating knee kinematics precisely in vivo , the tests were carried out under artificial conditions as outlined above.
Gravimetric measurements: wear and tear on the PE inlays was assessed by measuring its weight using a precision scale (accuracy: ±10µg) (Satorius, Göttingen) according to the ISO 14243-2 standard. Identical control components were used to control for the amount of fluid absorbed by the PE .
Surface inspection: The components of the prosthesis were photographed and examined under a scanning electron microscope (Leica S440i
).
|
The extensive tests performed by IMA GmbH in Dresden did not yield any surprises, instead they fully confirmed the predictions.
|
Testing device MTS
Minibionix 858 |
|
Forces and movements in the testing devic |
Axial rotation and AP translation during a gait cycle in the testing device Minibionix 858 (left) and the anterior/posterior forces and axial torque in the Instron-Stanmore KS4 (right)
|
The ÆQUOS G1 underwent an AP translation of up to 14 mm during the tests.
The testing device Instron-Stanmore KS4 does not cause a roll back by itself. In as much as a roll back is detectable (14 mm for the ÆQUOS G1), it is caused by the artifical joint itself.
It is important to note that the testing device Minibionix does not permit the artificial joint to roll without constraint, forcing the joint to carry out a certain level of sliding motion instead. As a result the ÆQUOS G1 is not expected to fully exploit the advantages associated with rolling, increasing the wear and tear of the tibial inlays and tending to yield more conservative estimates for the durability.
The tests involved flexion/extension in not only isolation, but also axial rotation. |
The peak axial load on the joint is about 2200N during the simulated gait cycle. Flexion is about 20 deg during a cycle.
. |
|
Gravimetric measurements: the joints TKR 19, 20 and 21 suffered a loss between 8.5 and 13.3 mg/10 6 cycles. The loss of mass was reduced to about 7.5 mg/10 6 cycles after the first 2 million cycles, suggesting that after the joint pairs are broken in, they roll and slide on each other more smoothly.
Axial rotation was not applied in the TKR 19 joint for the first 2 million cycles of flexion/extension. In that case, no loss of mass was detectable. It only became appreciable after the axial rotation was also switched on.
These data demonstrate that rolling is the most dominant and conservative form of motion for flexions up to 20 deg for the ÆQUOS G1 joint. The results of wear and tear are excellent in comparison with other knee joints on the market. |
 |
Surface inspection: The tibial inlays revealed medially and laterally clearly circumscribed contact areas, with a smooth and shiny reflection of the UHMWPE. Three small troughs could be detected, which are probably the result of the three peak loads during the gait cycle.
This waviness is absent in conventional prostheses because the centers of the contact surfaces do not shift on the tibial plateau (Walker et al., Giddings et al.)
The images of the scanning electron microscope confirm that the surface is smooth and the presence of a sharp border with the milling pattern.
The tibial contact areas of the TKR22 was A l = 203,1mm² on the lateral side and Am = 269,1mm² on the medial side. These values are comparable with the results from the pressure-sensitive films.
|
| |
Aequos tibial inlay after 5 million cycles. The eminentia intercondylaris and its surrounding areas including the fossa are highly polished as a result of the rolling.
|
|
|
Electronmicroscopic image of the tibial inlay shown above. The smooth surface is sharply distinct from the milling pattern. Only a few small and isolated particles were detectable.
|
Conclusion: the ÆQUOS G1, with its natural kinematics, has excellent tribological test scores. No wear and tear was detectable for pure flexion/extension without axial rotation. The wear and tear when both movements are permitted is very small (7.5 mg/10 6 cycles). This low level of wear and tear is a result of the joint running extremely smoothly after an initial breaking-in period.
At first glance, these results are surprising, given that one would expect a slight increase in wear and tear in the lateral TFJ because of the convex-concave surface geometry. However, as a result of the fact that the prosthesis experiences little friction by its very design, this disadvantage is more than offset and the wear and tear is in fact reduced.
The surfaces of the tibial joints confirm that the gear system undergoes a breaking-in phase. These contact surfaces correspond to the roll back. In this manner, rolling occurs under loads using an extensive roll back as the predominant type of motion.
Additional tests, using an Oxford Rick device, have also demonstrated that the ÆQUOS G1 carries out rolling, followed by sliding motions (Prof. Thomsen und Dr. Li; Heidelberg).
Preliminary radiological in vivo studies have also confirmed the roll back of the ÆQUOS G1 joint (Prof. Stürmer, University Hospital Göttingen.
Rolling under loads also yields the following benefits:
|
|
The tibial plateau and the interface with the bone are loaded exclusively by forces that are perpendicular to the surface during peak loads.
There is neither any static friction when starting from rest, nor any sliding friction during movements. Taken together, the degenerative effects of friction and shearing forces are kept at a minimum, ensuring superior durability and a high degree of stability. |
The ÆQUOS G1 joint permits abduction and adduction because the contact points lie close to the eminentia intercondylaris leaving the natural link quadrangle in this region intact.
|
 |
The benefits for the patient
The “natural” motion of the ÆQUOS G1 joint ideally combines flexion/extension, axial rotation and abduction/adduction. The principle, “rolling followed by sliding”, is the basis for movements characterized by a very high degree of stability and extremely low levels of wear and tear.
Because the movements of the implanted joint are so similar to the natural case, the patient quickly becomes comfortable with the replaced knee joint and rapidly regains mobility without the frustrating experience of having to relearn walking.
Climbing stairs and walking on uneven terrain do not pose a problem for patients with an ÆQUOS G1 implant.
The ÆQUOS G1 joint does without auxiliary constructions (studs, screws, mobile bearings etc), which facilitates safe bone resection without complications. The design makes it easier for the surgeon to align the tibial plateau axially and the femoral head laterally, safeguarding the quality of the surgery.
The advantages and benefits for the patient are truly impressive and have been amply documented in a large number of surgeries and longitudinal studies.
|
|
|

